Many people don’t realize that several common over-the-counter medications and prescriptions can negatively interact with alcohol or other street drugs they may be using. If you aren’t careful about recreational or prescription drug use, you can experience potentially dangerous drug interactions.
Pharmacists and doctors attempt to control unwanted drug combinations by carefully monitoring each patient’s prescriptions. However, if you’re using illegal substances, you may not be aware of the potential risks of mixing those drugs with prescribed or OTC medications. The same can be said of mixing alcohol with certain prescription drugs or illicit substances.
Common Drug Interactions That Can Be Dangerous
Opioids, benzodiazepines, and alcohol can cause dangerous side effects and interactions, especially when they’re taken together or in combination with unregulated doses of street drugs. Here are the most common dangerous drug interactions.
Vicodin and Xanax
Vicodin, a prescription opioid that contains both acetaminophen and hydrocodone, can cause dangerous, even life-threatening side effects when combined with benzodiazepines like Xanax.
When taken separately, both opioids and benzodiazepines carry a risk of respiratory suppression and overdose if you take too much. When taken together, even in their prescribed amounts, the combined sedative effects on the respiratory system can be deadly. A 2016 cohort study revealed that people who were prescribed both opioids and benzodiazepines were 10 times more likely to die of an overdose than people who were prescribed opioids alone [1].
Combining these drugs can also cause severe cognitive impairments and contribute to deadly accidents and serious bodily injuries. It’s important to talk to your doctor about potential interactions between prescription opioids and benzodiazepines.
Opioids and Alcohol
One of the most common and serious side effects of opioid usage is sedation and impaired breathing. When an opioid is combined with a central nervous system depressant like alcohol, the potential for deadly respiratory depression is significantly higher than when opioids are taken alone.
In a study of alcohol-related deaths in 2020, alcohol was found to be a contributing factor in over 17% of deaths caused by opioid overdose [2].
Benzodiazepines and Alcohol
Benzodiazepines like Valium, Xanax, and Klonopin are central nervous system depressants that are used to treat anxiety disorders, insomnia, seizures, and muscle spasms. Like all depressants, benzodiazepines slow down activity in the brain and nervous system, which can in turn cause slow, shallow, or irregular breathing. Combining even prescribed doses of benzodiazepines with alcohol can cause overdose and death from severe respiratory depression.
In one study of alcohol-related overdose deaths, the benzodiazepine Tamazepam was found to lower the threshold for alcohol overdose by nearly 20% when compared to overdoses caused by alcohol alone [3].
Opioid Maintenance Therapy Drugs and Benzodiazepines or Alcohol
Many people who suffer from substance use disorders have co-occurring mental health conditions like anxiety and depression. For people taking suboxone or methadone to manage an opioid use disorder, it can be dangerous to take benzodiazepines for anxiety or to self-medicate mental health issues with alcohol.
Medicated-assisted therapy (MAT) drugs like Suboxone (a combination of buprenorphine and naloxone) and Methadone (a long-acting full opioid agonist) can slow down central nervous system activity. When combined with sedative drugs like benzodiazepines (which are often used to treat short-term anxiety), there is a risk of dangerous respiratory depression and overdose death. The same is true of combining MAT drugs with depressants like alcohol.
It’s critical to talk with your doctor about your prescriptions and to work together to assess your risk level and address your concerns.
Opioids and Potentiators
Some people mix opioids with over-the-counter substances to produce feel-good endorphins. Even orange and grapefruit juice may increase the effects of oxycodone.
Many people combine antihistamines, sleeping medications, and nausea medications with opioids to increase their effects. Even the herb St. John’s wort enhances the effects of opioids.
Taking opioids with potentiators leads to unpredictable and potentially deadly side effects. It can also exacerbate substance abuse issues and increase the likelihood of drug dependency.
Professional Help for Substance Abuse and Alcohol Addiction
If you’re suffering from an addiction to opioids, alcohol, or benzodiazepines, you are at risk of life-threatening side effects when you combine these drugs with other illicit substances or prescription medications. Addiction can drive irrational behaviors and decision-making that puts your health and safety at risk. In addition to overdose risk, drug interactions can cause coma, heart attack, seizures, and other negative side effects.
You don’t have to remain in the cycle of addiction. If you’re experiencing drug or alcohol dependency, the first step to getting clean and rebuilding your life is to find an addiction treatment program that works for you.
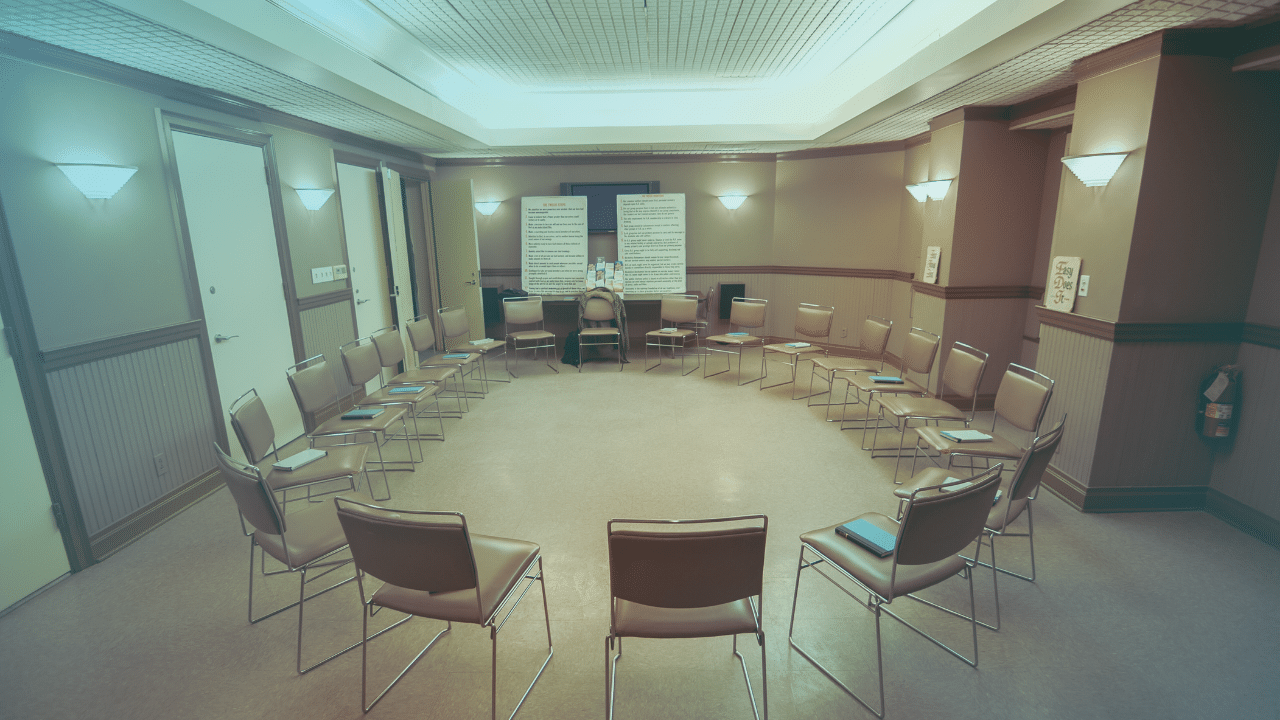
STR Behavioral Health provides safe detox and holistic addiction treatment for substance use disorder, alcohol use disorder, and dual diagnosis in Pennsylvania.
Our addiction programs span multiple levels of care so you find the treatment model that works with your life and recovery goals:
- Safe, medically supervised detox
- Residential addiction treatment program
- Intensive outpatient program
- Partial hospitalization program
- Outpatient addiction treatment
Explore our locations and reach out today to get the help you need in a supportive, caring environment.
Sources:
- Dasgupta, Nabarun, et al. “Cohort Study of the Impact of High-Dose Opioid Analgesics on Overdose Mortality.” Pain Medicine, Aug. 2015, p. n/a-n/a, https://doi.org/10.1111/pme.12907.
- White, Aaron M., et al. “Alcohol-Related Deaths during the COVID-19 Pandemic.” JAMA, vol. 327, no. 17, 18 Mar. 2022, pp. 1704–1706, jamanetwork.com/journals/jama/fullarticle/2790491, https://doi.org/10.1001/jama.2022.4308.
- Koski, Anna, et al. “Alcohol and Benzodiazepines in Fatal Poisonings.” Alcoholism: Clinical and Experimental Research, vol. 26, no. 7, July 2002, pp. 956–959
Explore this article:
Explore Our Facilities
Drug and alcohol detox and residential treatment for addiction and mental health disorders
Outpatient treatment center for substance use disorder and mental health disorders
Outpatient treatment center for substance use disorder and co-occurring mental health disorders